For many people, antidepressants can be life changing. But for others, the relief never quite comes or it fades too soon. When this happens, it’s easy to wonder: Why isn’t my antidepressant medication working?
The truth is that depression isn’t a one-size-fits-all condition. And neither are its treatments.
Major depressive disorder affects the brain in complex, individual ways. Sometimes, the neural circuits involved in mood regulation need a different kind of support beyond medication.
At Clear Path Psychiatry, we specialize in helping people find relief when traditional options do not provide enough benefit.
One of the most effective next-step options is Transcranial Magnetic Stimulation (TMS), a non-invasive therapy that helps the brain heal by stimulating the circuits involved in mood regulation.
How Do Antidepressant Medications Work?
Antidepressants remain one of the most widely prescribed treatments for depression.
These medications work by adjusting the levels and activity of neurotransmitters, the chemical messengers such as serotonin, norepinephrine, and dopamine that influence mood, motivation, and emotional regulation.
For many people, this approach is effective. Increasing serotonin availability, for instance, can help restore balance, improve sleep, and ease the weight of persistent sadness.
However, the brain is extraordinarily complex. Depression isn't caused by a simple chemical deficiency, and antidepressants affect the entire body's neurochemistry rather than only the specific brain circuits that have gone quiet.
This is one reason it often takes 4 to 6 weeks before any noticeable change occurs, and why some people cycle through multiple medications without finding one that works.
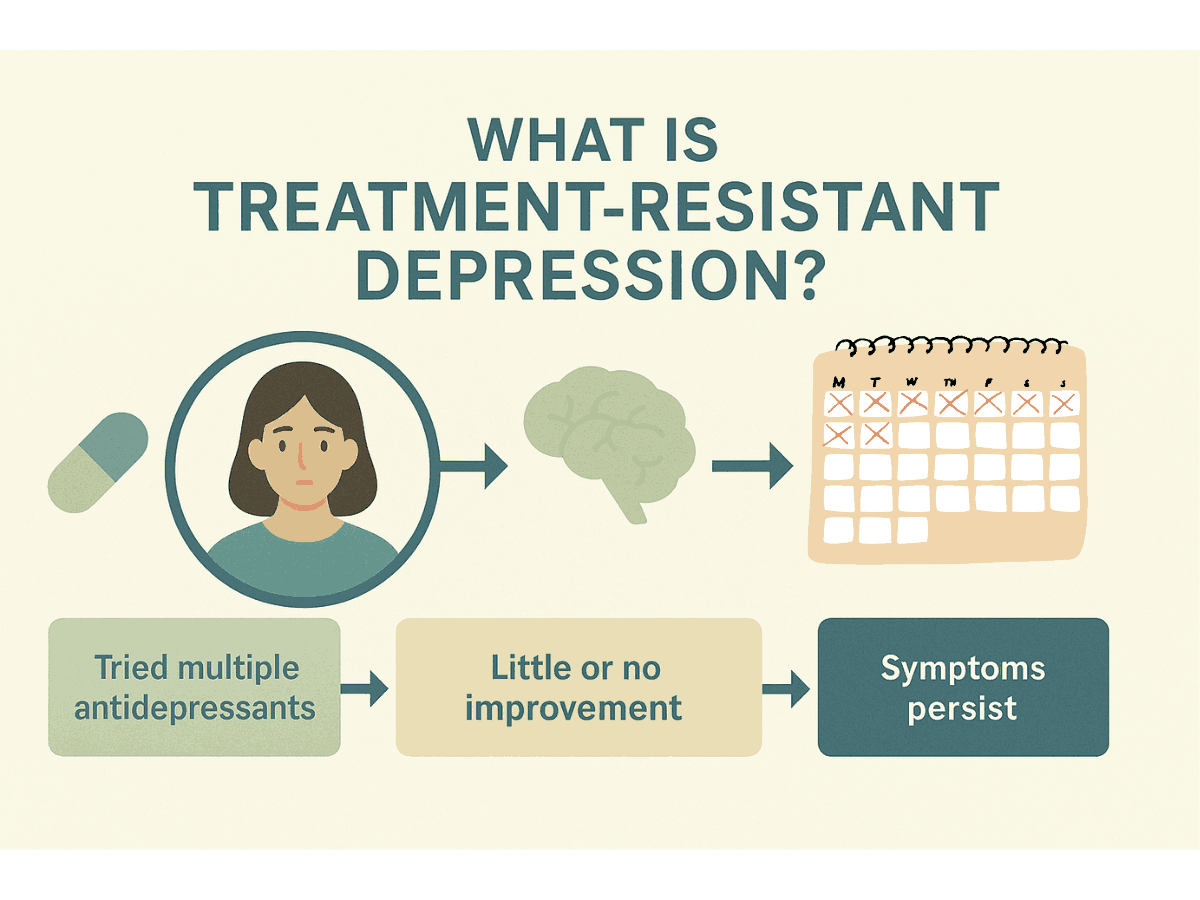
Research shows that approximately 30% of people with major depressive disorder don't experience adequate symptom relief after trying two or more antidepressants, a condition known as treatment-resistant depression.
For these individuals, the issue isn't willpower or patience. Their neural pathways may simply require a more direct intervention instead of another chemical adjustment.
How Does TMS Work Differently Than Antidepressants?
Transcranial Magnetic Stimulation (TMS) takes a fundamentally different approach to treating depression.
Instead of relying on medication to influence brain chemistry, TMS directly stimulates the specific neural circuits that regulate mood and motivation.
Using focused magnetic pulses that are similar in strength to those used in an MRI, TMS targets the left dorsolateral prefrontal cortex, a region that often becomes underactive in depression.
These gentle pulses activate neurons and encourage them to fire and reconnect with other mood-regulating areas, such as the limbic system, helping restore healthy communication patterns.
We can think of it this way: when depression causes certain brain networks to go offline, antidepressants try to coax them back through chemistry, while TMS flips the switch directly.
n other words, antidepressants work on the messengers, and TMS works on the messaging system itself.
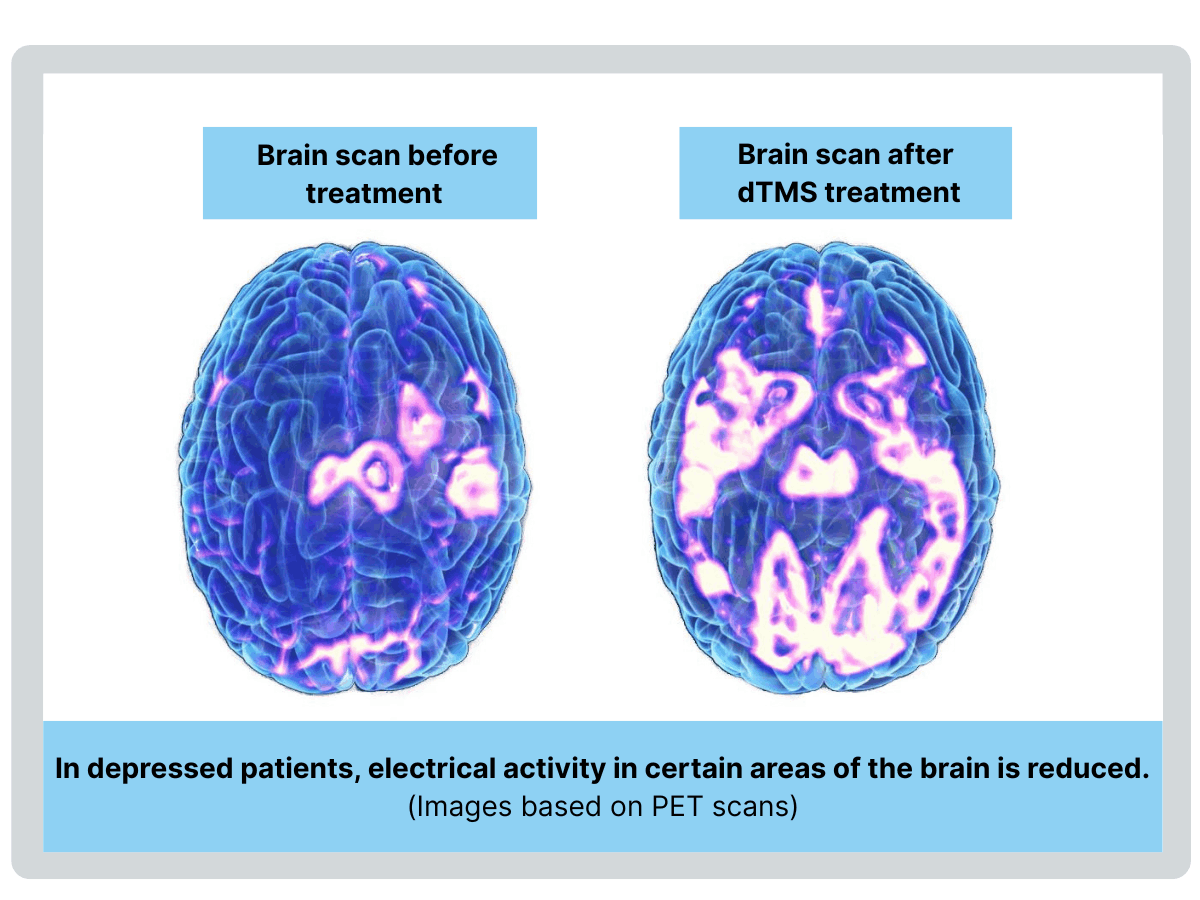
Over the course of treatment, this repeated stimulation strengthens synaptic connections, essentially retraining the brain to maintain healthier patterns of activity. The improvements are visible on brain imaging scans, and research shows they often remain long after treatment ends.
TMS is completely non-invasive, does not require anesthesia, and causes no systemic side effects.
During each session, you remain fully awake and comfortably seated in a chair while wearing a helmet that delivers targeted pulses that feel like gentle tapping on the scalp.
Some people describe the sensation as a light woodpecker or rhythmic pressure.
Sessions typically last three to twenty minutes, depending on the treatment protocol. There is no sedation and no downtime. You can drive yourself home, head to work, or resume your normal routine immediately afterward.
The most common side effect is mild scalp tenderness or headache that usually resolves quickly. These sensations tend to lessen as the brain adjusts and usually do not interfere with daily activities.
Unlike antidepressant medications, TMS does not cause systemic side effects that often make medication difficult to tolerate, such as weight gain, grogginess, or sexual dysfunction.
Most people can continue working, driving, exercising, and engaging fully in life while completing their treatment course.
Because it is so well tolerated, TMS has become a preferred alternative for many people who want a non-invasive, medication-free option for treating depression.
Why Do Some Brains Respond Differently?
Depression doesn't look the same on a brain scan for everyone.
Functional MRI studies reveal that some people have reduced activity in the prefrontal cortex, others show overactivity in fear-processing regions such as the amygdala, and still others have disrupted communication between entire brain networks.
This variability helps explain why antidepressants and other treatments work differently from one person to another.
Every brain processes chemistry and electrical signals in its own unique way.
Genetics matter.
Variations in genes that influence how your body metabolizes medication, such as the CYP450 enzyme family, can determine how well antidepressants are absorbed and processed. Genetic testing can sometimes identify these issues, although the science is still evolving.
Brain structure matters.
Depression that co-occurs with chronic stress, inflammation or a history of trauma may involve circuits that medication can’t directly reach. If the prefrontal cortex, the brain's "executive center", has essentially powered down, chemical messages may have nowhere to land. TMS directly stimulates these regions, helping restore healthy signaling even when medication has not helped in the past.
Symptom patterns matter.
Not all depression presents the same way. People with symptoms of cognitive slowing (brain fog or difficulty concentrating), loss of pleasure or motivation, or depression that developed after trauma often respond particularly well to TMS.
This is why TMS can succeed where medication has not: it bypasses the chemistry and directly reactivates the circuits that have stopped communicating.
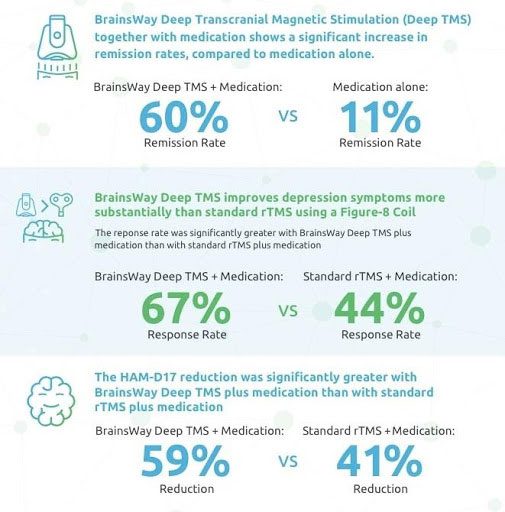
In clinical trials, 50-60% of people with treatment-resistant depression experience significant symptom reduction with TMS, and about one-third reach full remission. See here.
Can TMS and Antidepressants Complement One Another?
It doesn’t have to be either/or.
Many of our patients continue their antidepressant medication while receiving TMS therapy.
Some find that TMS helps their medication work more effectively or allows them to gradually reduce their dose under their provider’s supervision.
Others discover that the combination provides greater symptom relief than either treatment alone.
We also see TMS restore responsiveness to other forms of care.
When the brain’s mood circuits begin functioning again, therapy becomes more effective, cognitive-behavioral strategies start to “stick,” mindfulness practices feel less overwhelming, and and even everyday activities like exercise begin to feel rewarding again.
A personalized plan may include:
TMS sessions combined with ongoing coordination with your existing therapist and/or prescribing provider for medication management
Regular follow-up appointments with your Clear Path provider to monitor progress, discuss your experience, and adjust treatment settings as needed
Lifestyle recommendations that support brain health, including healthy sleep habits, movement, and nutrition
Follow-up or maintenance TMS sessions if needed to sustain long-term results
At Clear Path Psychiatry, every plan is created individually.
We consider your medical history, symptoms, and treatment goals to build a path that truly fits you.
Our goal is not just to manage depression but to help you feel supported, understood, and more like yourself again.
What Can I Expect During TMS Treatment?
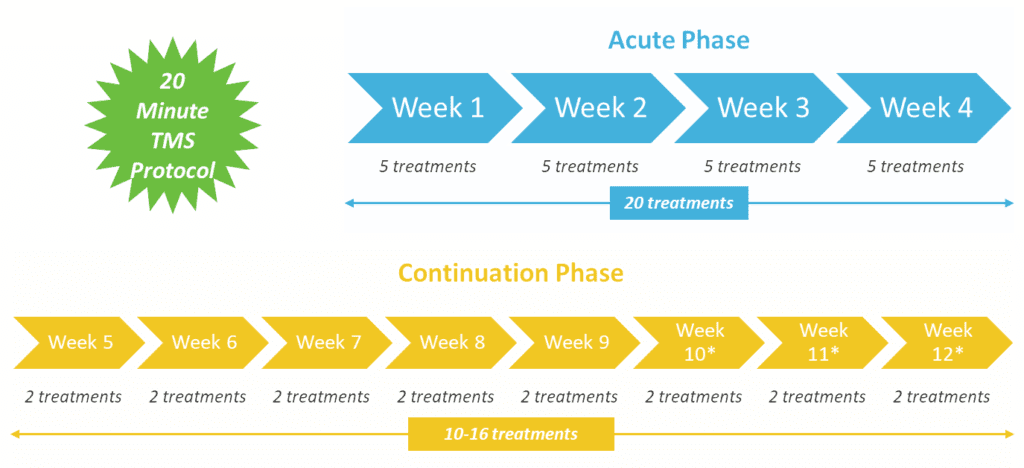
Standard BrainsWay® Deep TMS FDA-Approved Protocol:
For Major Depressive Disorder, it is most common to have five sessions a week, followed by an 8 to 12-week continuation phase with two sessions a week.
Each session includes about 20 minutes of active stimulation (although some protocols are as little as 3 minutes)
Timeline for improvement:
Most people notice subtle shifts within the first few weeks. Morning mood may start to feel a little lighter, motivation begins to return, and concentration gradually improves. By weeks 4 or 5, these changes often become more noticeable. Progress builds gradually, reflecting the brain’s process of creating new, healthier communication pathways.
Your provider tracks your progress throughout treatment using standardized depression scales such as the PHQ-9 to ensure that the protocol is working effectively and to adjust if needed.
Your treatment space:
Each session takes place in a private, comfortable room designed for calm and focus. With some protocols lasting only a few minutes, many patients choose to simply sit quietly during their session, while others listen to music, read, or meditate.
Accelerated TMS protocols:
For select patients, we offer accelerated treatment options that condense the full course of TMS into a shorter timeframe, sometimes as brief as one to five days with multiple sessions per day. These protocols can be particularly helpful for those who can't commit to daily appointments for four weeks, or who need faster relief from symptoms. Although accelerated TMS protocols are not yet covered by all insurance plans, we'll walk through the costs openly during your consultation and help you decide whether this condensed approach is the right fit for your situation.
One type of Accelerated TMS protocol:
See our other blog posts about Accelerated dTMS:
Can Depression Be Treated in a Single Day?
The Benefit of Accelerated TMS Protocols
What is the Science Behind Deep TMS?
TMS works through a principle called electromagnetic induction, where a rapidly changing magnetic field generates a small electrical current in nearby neurons, causing them to fire.
This process helps underactive brain regions “wake up” and reestablish communication with the rest of the mood network.
At Clear Path Psychiatry, we use the BrainsWay® Deep TMS system that utilizes a magnetic field of approximately 1.5-2 Tesla, comparable to a standard MRI machine, but it is carefully focused on a specific region a few centimeters beneath the scalp.
This precision is what makes TMS both safe and effective: it targets mood circuits directly without stimulating the entire brain.
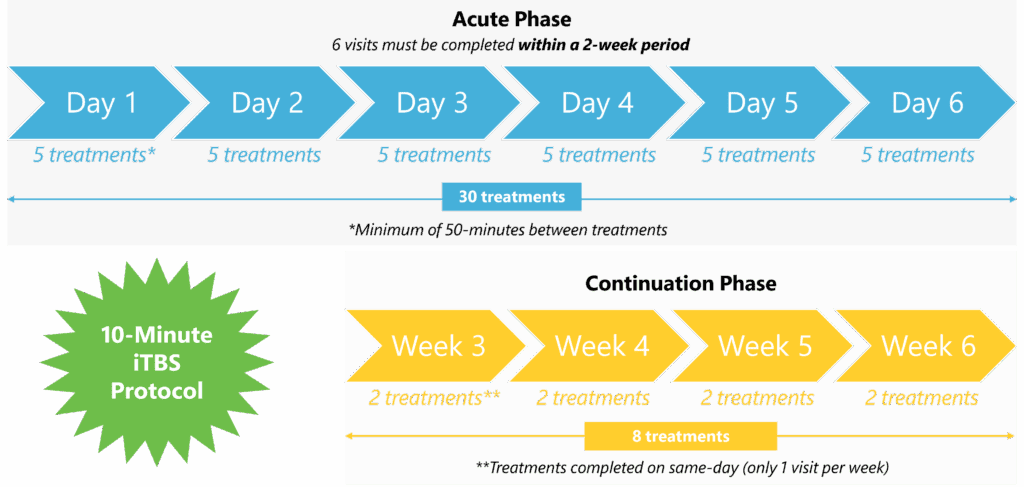
Deep TMS technology:
The BrainsWay® Deep TMS system employs a patented H-coil design capable of reaching deeper and broader brain regions than traditional figure-8 coils.
This advanced technology is FDA-cleared for both major depressive disorder (MDD) and obsessive-compulsive disorder (OCD).
Research suggests that this deeper stimulation may be particularly effective for treatment-resistant depression, where standard antidepressant medications have not brought relief.
How it creates lasting change:
Repeated stimulation strengthens synaptic connections through a process called long-term potentiation, often summarized by the phrase, “neurons that fire together, wire together.”
Over time, this process builds more resilient neural pathways that support mood regulation even after the treatment course has ended.
Clinical studies show that many patients maintain significant improvement for a year or longer following Deep TMS.
Safety profile:
TMS has been used safely in hundreds of thousands of patients worldwide.
The most serious potential risk, seizure, is extremely rare, occurring in approximately 0.1% of patients, which is similar to the seizure risk associated with antidepressant medications.
The most common side effect is mild scalp discomfort or headache during or shortly after sessions, which typically improves within the first week as your body adjusts to treatment.
See our blog post about dTMS:
Getting to Know BrainsWay® Deep TMS
Who is TMS For?
You may be a good candidate for TMS if:
You have tried 2 or more antidepressant medications without adequate relief
You have medical or psychiatric factors that make medication management complicated|
Medication side effects have been difficult or intolerable
You want to reduce your reliance on medication or explore remission without medication
TMS may not be appropriate if:
You have metal implants in or around your head (excluding titanium dental fillings)
You have a history of seizures or certain neurological conditions
You are currently in crisis or need a higher level of care before starting outpatient treatment
Every situation is unique. During your consultation, we will review your medical history, goals, and current symptoms to determine whether TMS is a safe and effective next step for you.
Is TMS A New Way Forward For Treating Depression?
If medication hasn't brought the relief you hoped for, you haven't run out of options. You may have simply reached the point where a more targeted brain-based approach makes sense.
TMS offers that opportunity.
It is a treatment that works directly on the brain circuits involved in depression, with a strong evidence base, minimal side effects, and results that can last long after the final session.
Clear Path Psychiatry specializes in TMS for depression, anxiety, and OCD, using the most advanced technology in a calm, supportive environment where you are truly seen and cared for.
Our team will guide you through every step, from your initial consultation to your final session and beyond.
How Do I Get Started with TMS?
Starting TMS can feel like a big step, but you will not be doing it alone. Here’s what the process looks like and how we’ll support you along the way:
- Initial consultation –
We review your history, current symptoms, past treatments, and goals. We will explain exactly how TMS works and answer all of your questions. - Insurance verification –
Our team handles prior authorization and helps you understand coverage. Most major insurance plans cover standard TMS protocols for treatment-resistant depression, anxiety with depression and OCD. - Treatment planning –
We create your treatment schedule around your life and discuss what to expect during each phase. - Ongoing support –
Throughout treatment and afterward, we monitor your progress and make adjustments as needed. You will have regular follow-ups with your provider to review your progress, discuss any changes, and ensure your treatment remains both comfortable and effective.
Depression can feel isolating. Treatment shouldn't.
We're here to walk with you through every step toward healing.
If you’re ready to explore an approach that works differently, we invite you to take the next step...
Ready to learn whether TMS might be right for you?
Reviewed by Eliza Brink, DNP, PMHNP-BC